clinical facilitation 101
A blended learning course for registered nurses aimed at developing leadership skills and gaining a basic understanding of bedside mentorship.
MY ROLE
IDEATION
I partnered with three stakeholders and an associate nurse educator to uncover insights and translate these into a curriculum outline that addressed learner confidence, student nurse needs and organisational demands.
STRATEGY & VISION
I created frameworks and prototypes to share the vision, curriculum content and project plan. I evangelised learner goals and balanced organisational and external stakeholder goals. I prioritised and negotiated essential-only content to create a minimum viable product for future testing and iteration.
DESIGN EXECUTION & VALIDATION
I designed the curriculum and built out the content into session plans that utilised face-to-face facilitation, short videos, group & individual activities/discussions, audio podcasts, article discussions and drip-fed emails for reflection.
I arranged small groups of up to three facilitators to participate in the learning as a prototype before delivering the curriculum to forty participants in one day. I surveyed each participant prior to commencing the course, at the end of the course and one month after completing the course.
LEADERSHIP
I presented the curriculum plan to university academics and organisational leaders to gain buy-in throughout the project lifecycle.
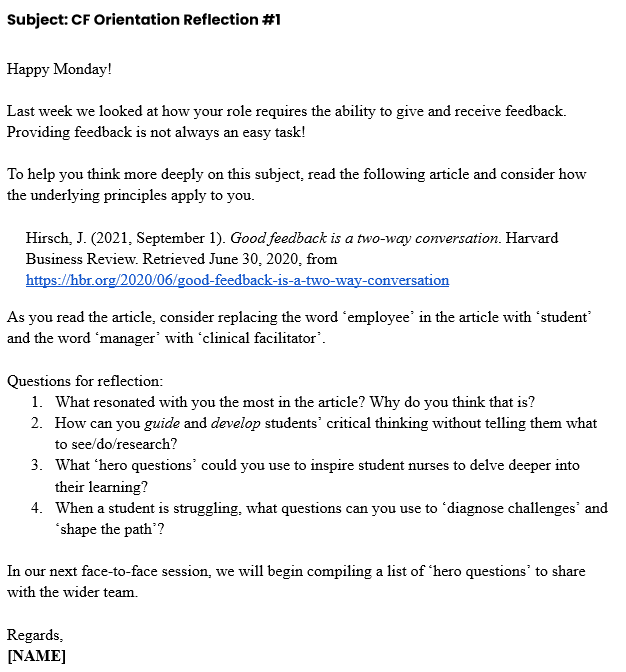
Example of a drip-feed email developed for ‘thought prompts’ that scaffolded knowledge from previous sessions and prepared the learner for future sessions.
THE CHALLENGE
IMPROVE EFFICIENCY IN STUDENT NURSE FACILITATION AND ASSESSMENT AMONG CLINICAL FACILITATORS
The Entry to Practice Team is a team of Clinical Facilitators (Registered Nurses) who facilitate learning for student nurses who are completing a clinical placement in any of the clinical areas within the hospital. No formal training in education or educational theory is required for the role. However, the Clinical Facilitators are expected to assess each student on their performance against national standards, identify underperforming students, and provide tailored teaching support.
Research articles identified a recurring problem with clinical facilitators expressing a sense of overwhelm with their role due to a lack of preparation for teaching and mentorship.
I wanted to solve this problem because the clinical facilitation team voiced similar concerns for new staff members and the added burden on senior staff. The universities (external stakeholders) also expressed concerns about the quality of teaching for students on placement and a lack of evidence of student learning and support when students were deemed unsuccessful during their placements.
I set out to develop an Australia-first curriculum to increase confidence levels in teaching and mentorship among clinical facilitators and improve the student nurse experience in learning and support while on clinical placement.
THE FRAMEWORK
HOW WE GOT THERE
I followed the ADDIE methodology (Analyse, Design, Develop, Implement and Evaluate) to develop a curriculum solution that solved the identified problems. I eventually created a curriculum that senior leadership could deliver virtually and face-to-face or a blended program.
I ran discovery sessions with the clinical facilitators – one session interviewed senior clinical facilitators, and the other session interviewed the team’s newest members. These sessions focused on analysing the facilitators’ perceptions of what they wish they had known when starting in the position versus what they knew now.
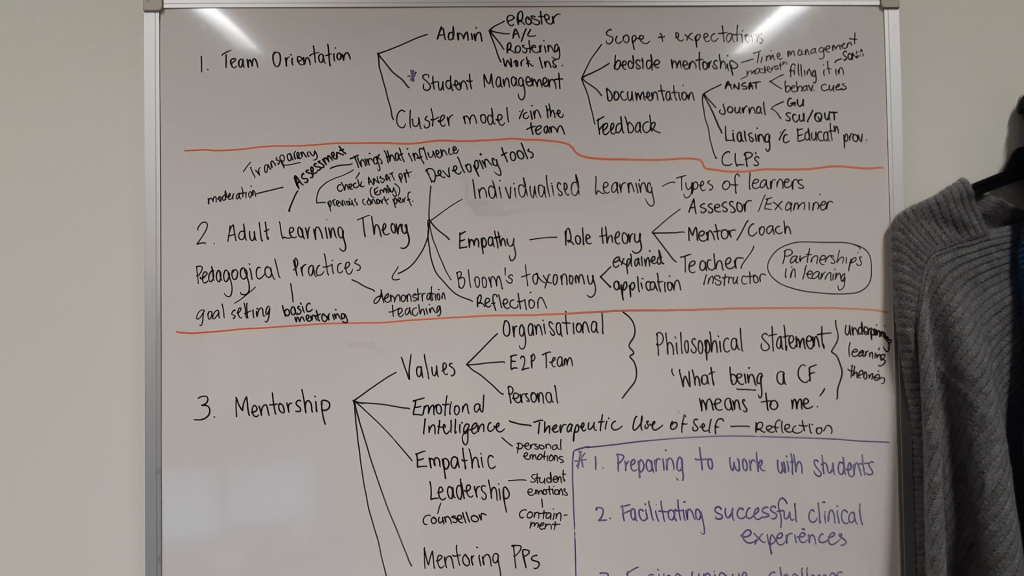
The early content brainstorming session where conten topics began to take shape as lessons and modules.
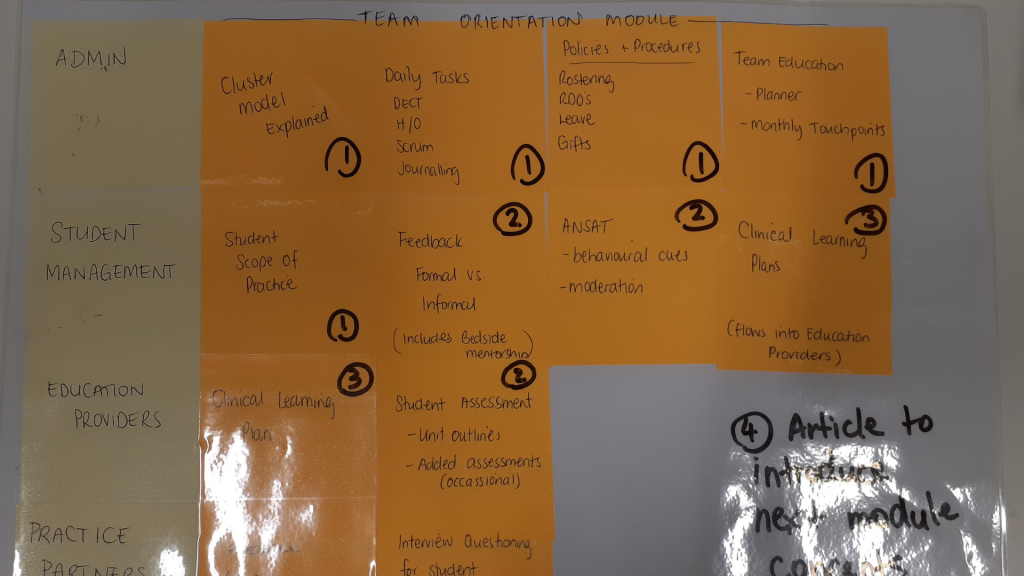
A completed card sorting activity used to identify and arrange essential information into course modules.
I also engaged the local universities to understand their expectations of how a competent clinical facilitator should demonstrate knowledge and skill in teaching the students they send to the hospital for clinical placement.
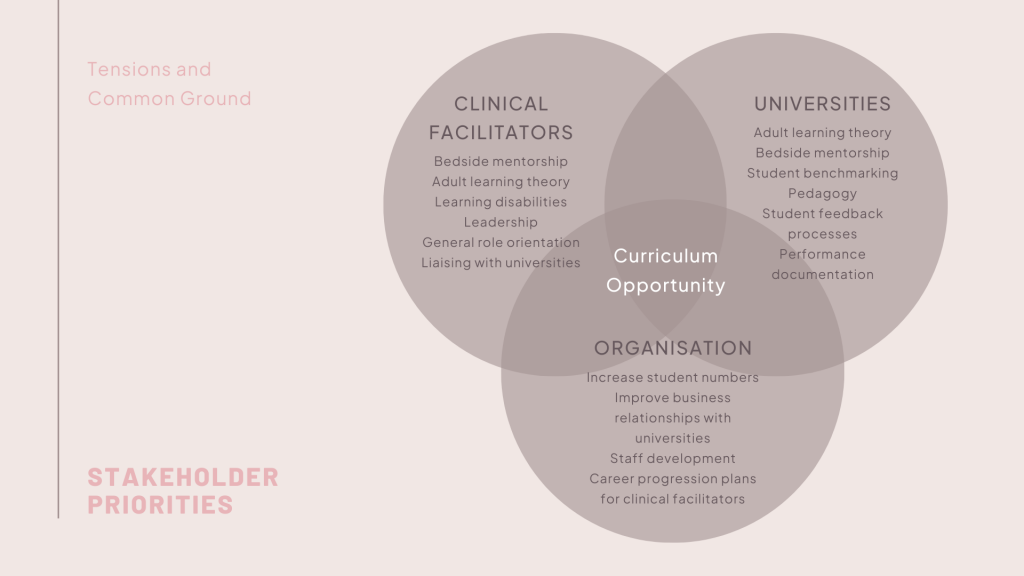
“The combination of external and internal stakeholders created a unique environment where competing priorities added an extra layer of complexity.”
The project faced several challenges which included:
- The clinical facilitation team had limited time to attend face-to-face training due to the continuous rotation of student nurses throughout the hospital.
- The clinical facilitation team experienced chronic staff shortages during the COVID-19 pandemic impacting access to learners during research, design and implementation phases. In addition, the organisation reduced the time allowed for training once the staff member had commenced with the team.
- Three main stakeholders were identified: clinical facilitators, the organisation, and the universities that send students on placement to the facility. The combination of external and internal stakeholders created a unique environment where competing priorities added an extra layer of complexity.
- Delivering an end product on the organisation LMS will take approximately 1 – 2 years due to the small size of the Learning & Development team.
- The immediate resources available to produce the course were limited and consisted of Microsoft Office applications.
THE SOLUTION
INTRODUCING A NEW STANDARD OF CLINICAL FACILITATION
The final package consisted of three modules and followed a blended model using a printed workbook, email prompts and face-to-face workshops.
The first module became a general orientation to the team which was given on the facilitator’s first day. This module included face-to-face learning and ‘on-the-job’ training with a senior staff member where the employee would ‘shadow’ them. I developed session plans for the face-to-face workshops so that anyone could pick up the program and deliver it.
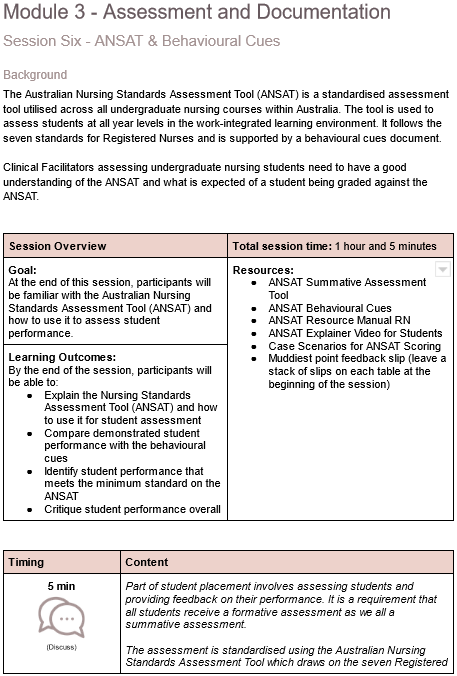
Example of a session outline developed for the third module.
The second module began to ease off in the delivery of face-to-face learning, representing a move from ‘hand holding’ the new facilitator to allowing them the space to develop their unique teaching style through experimentation with the course content. At this phase, the learner attends face-to-face sessions of no more than 1 hour at a time with drip-fed emails providing thought prompts for upcoming sessions.
The time limits were necessary given the lack of time for training available to the staff.
“Providing the course in this way enabled quick iterations according to feedback to upload a final version to the Learning Management System.”
The final module was delivered entirely online, and for the first cohort, it was delivered weekly via email. Providing the course in this way enabled quick iterations according to feedback to upload a final version to the Learning Management System.
The course is now in its second round with key components being converted to an online course using Articulate Rise, Articulate Storyline and Vyond animation as planned.
REFLECTIONS
WHAT I LEARNED
USING A DESIGN THINKING APPROACH CREATES FASTER BUY-IN
It was the first time I had used a design thinking framework in conjunction with ADDIE to develop a new curriculum. This approach was useful in managing the competing interests from each stakeholder as I was able to empathise with each of them on a much deeper level than before. I feel this contributed to the success of the project and gaining early buy in from all parties.
LEARNERS ENJOY COMMUNITY, NOT A FANCY LMS
Initially, I was disappointed with the software and technology available to create the end product; however, as I tested the course with the early users, it became evident that the content was much more critical. Building a community around the learning was much more important than prioritising the online development of the course.
Moving forward, I will now be looking for opportunities for participants to interact with other learners and create a sense of community despite it being a virtual learning experience.
Project Details
- Category: Curriculum development
- Date: 2020 - 2021
- Client: A local area health service
- Response: Loved it!
Project Attributes
- Curriculum development
- Instructional Design
- Face-to-face facilitation
- Session plan writing
- Email based learning (during iteration phase)
- Video editing
- Podcast development & voice over
- Workbook development
Software
- Microsoft Project
- Microsoft Outlook
- Microsoft Word
- Adobe inDesign
- Adobe PremierePro
- Adobe Audition
Project Details
- Category: Curriculum development
- Date: 2020 - 2021
- Client: A local area health service
- Response: Loved it!
Project Attributes
- Curriculum development
- Instructional Design
- Face-to-face facilitation
- Session plan writing
- Email based learning (during iteration phase)
- Video editing
- Podcast development & voice over
- Workbook development
Software
- Microsoft Project
- Microsoft Outlook
- Microsoft Word
- Adobe inDesign
- Adobe PremierePro
- Adobe Audition
MY ROLE
IDEATION
I partnered with three stakeholders and an associate nurse educator to uncover insights and translate these into a curriculum outline that addressed learner confidence, student nurse needs and organisational demands.
STRATEGY & VISION
I created frameworks and prototypes to share the vision, curriculum content and project plan. I evangelised learner goals and balanced organisational and external stakeholder goals. I prioritised and negotiated essential-only content to create a minimum viable product for future testing and iteration.
DESIGN EXECUTION & VALIDATION
I designed the curriculum and built out the content into session plans that utilised face-to-face facilitation, short videos, group & individual activities/discussions, audio podcasts, article discussions and drip-fed emails for reflection.
I arranged small groups of up to three facilitators to participate in the learning as a prototype before delivering the curriculum to forty participants in one day. I surveyed each participant prior to commencing the course, at the end of the course and one month after completing the course.
LEADERSHIP
I presented the curriculum plan to university academics and organisational leaders to gain buy-in throughout the project lifecycle.
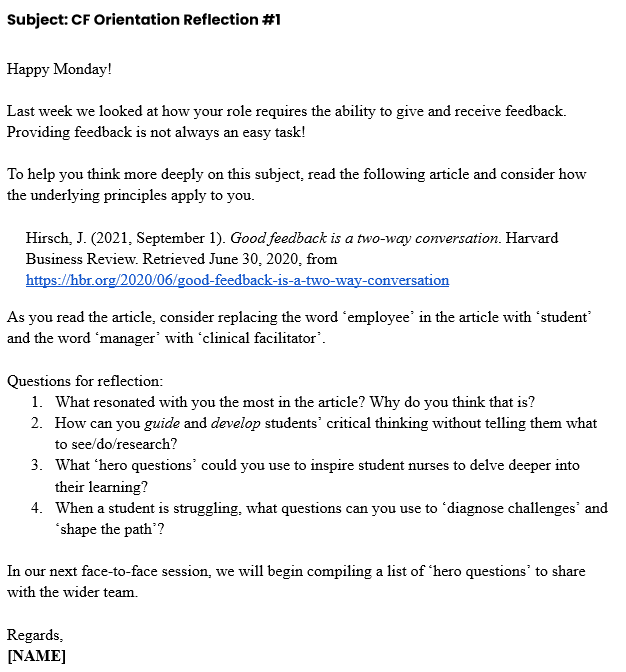
Example of a drip-feed email developed for ‘thought prompts’ that scaffolded knowledge from previous sessions and prepared the learner for future sessions.
THE CHALLENGE
IMPROVE EFFICIENCY IN STUDENT NURSE FACILITATION AND ASSESSMENT AMONG CLINICAL FACILITATORS
The Entry to Practice Team is a team of Clinical Facilitators (Registered Nurses) who facilitate learning for student nurses who are completing a clinical placement in any of the clinical areas within the hospital. No formal training in education or educational theory is required for the role. However, the Clinical Facilitators are expected to assess each student on their performance against national standards, identify underperforming students, and provide tailored teaching support.
Research articles identified a recurring problem with clinical facilitators expressing a sense of overwhelm with their role due to a lack of preparation for teaching and mentorship.
I wanted to solve this problem because the clinical facilitation team voiced similar concerns for new staff members and the added burden on senior staff. The universities (external stakeholders) also expressed concerns about the quality of teaching for students on placement and a lack of evidence of student learning and support when students were deemed unsuccessful during their placements.
I set out to develop an Australia-first curriculum to increase confidence levels in teaching and mentorship among clinical facilitators and improve the student nurse experience in learning and support while on clinical placement.
THE FRAMEWORK
HOW WE GOT THERE
I followed the ADDIE methodology (Analyse, Design, Develop, Implement and Evaluate) to develop a curriculum solution that solved the identified problems. I eventually created a curriculum that senior leadership could deliver virtually and face-to-face or a blended program.
I ran discovery sessions with the clinical facilitators – one session interviewed senior clinical facilitators, and the other session interviewed the team’s newest members. These sessions focused on analysing the facilitators’ perceptions of what they wish they had known when starting in the position versus what they knew now.
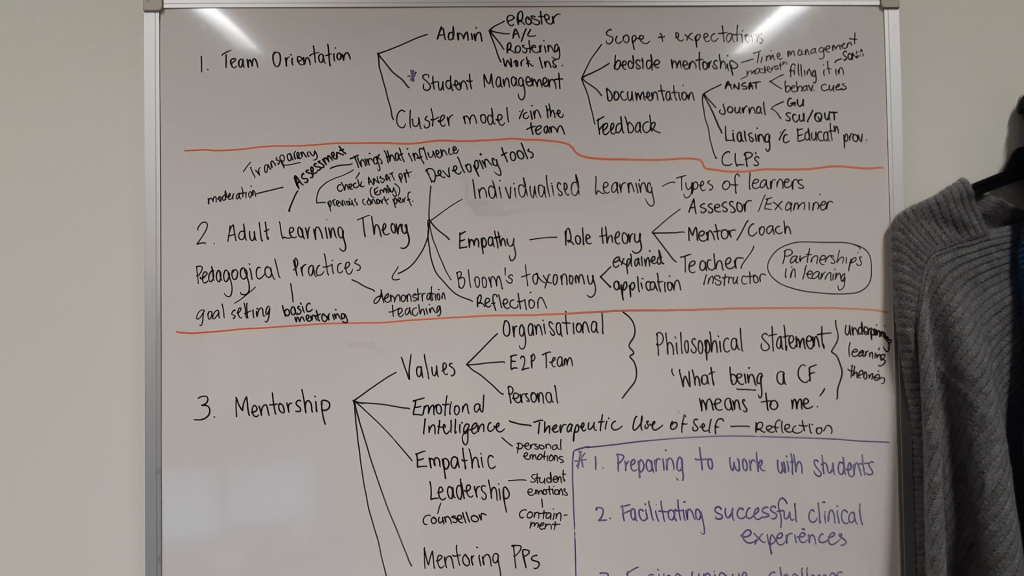
The early content brainstorming session where conten topics began to take shape as lessons and modules.
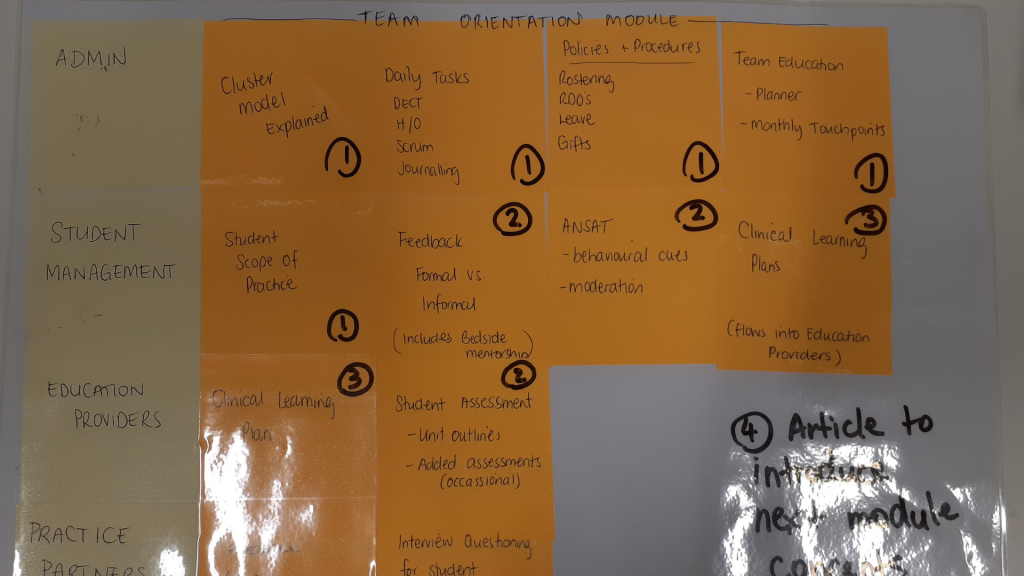
A completed card sorting activity used to identify and arrange essential information into course modules.
I also engaged the local universities to understand their expectations of how a competent clinical facilitator should demonstrate knowledge and skill in teaching the students they send to the hospital for clinical placement.
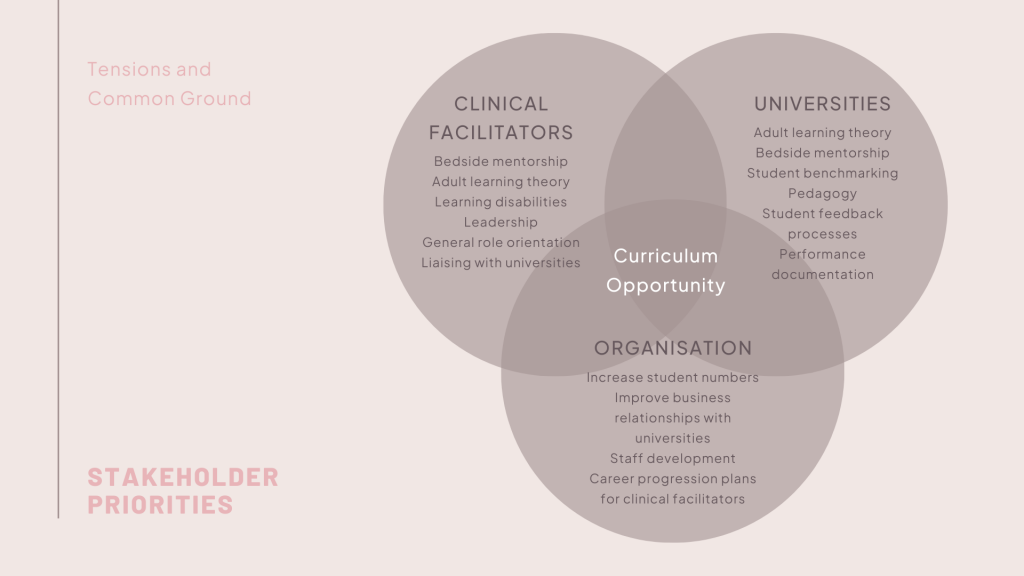
“The combination of external and internal stakeholders created a unique environment where competing priorities added an extra layer of complexity.”
The project faced several challenges which included:
- The clinical facilitation team had limited time to attend face-to-face training due to the continuous rotation of student nurses throughout the hospital.
- The clinical facilitation team experienced chronic staff shortages during the COVID-19 pandemic impacting access to learners during research, design and implementation phases. In addition, the organisation reduced the time allowed for training once the staff member had commenced with the team.
- Three main stakeholders were identified: clinical facilitators, the organisation, and the universities that send students on placement to the facility. The combination of external and internal stakeholders created a unique environment where competing priorities added an extra layer of complexity.
- Delivering an end product on the organisation LMS will take approximately 1 – 2 years due to the small size of the Learning & Development team.
- The immediate resources available to produce the course were limited and consisted of Microsoft Office applications.
THE SOLUTION
INTRODUCING A NEW STANDARD OF CLINICAL FACILITATION
The final package consisted of three modules and followed a blended model using a printed workbook, email prompts and face-to-face workshops.
The first module became a general orientation to the team which was given on the facilitator’s first day. This module included face-to-face learning and ‘on-the-job’ training with a senior staff member where the employee would ‘shadow’ them. I developed session plans for the face-to-face workshops so that anyone could pick up the program and deliver it.
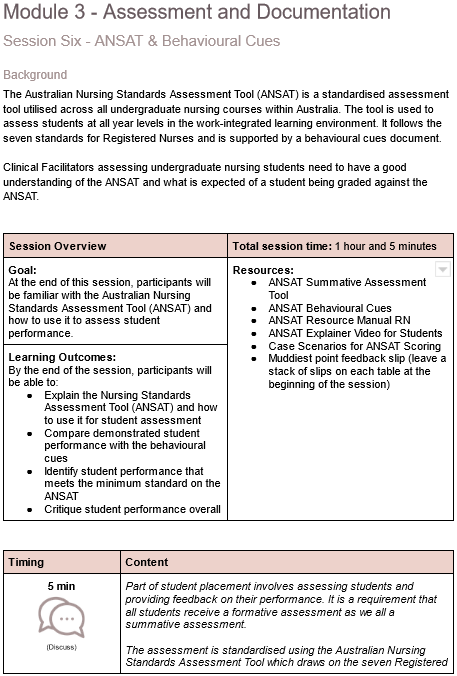
Example of a session outline developed for the third module.
The second module began to ease off in the delivery of face-to-face learning, representing a move from ‘hand holding’ the new facilitator to allowing them the space to develop their unique teaching style through experimentation with the course content. At this phase, the learner attends face-to-face sessions of no more than 1 hour at a time with drip-fed emails providing thought prompts for upcoming sessions.
The time limits were necessary given the lack of time for training available to the staff.
“Providing the course in this way enabled quick iterations according to feedback to upload a final version to the Learning Management System.”
The final module was delivered entirely online, and for the first cohort, it was delivered weekly via email. Providing the course in this way enabled quick iterations according to feedback to upload a final version to the Learning Management System.
The course is now in its second round with key components being converted to an online course using Articulate Rise, Articulate Storyline and Vyond animation as planned.
REFLECTIONS
WHAT I LEARNED
USING A DESIGN THINKING APPROACH CREATES FASTER BUY-IN
It was the first time I had used a design thinking framework in conjunction with ADDIE to develop a new curriculum. This approach was useful in managing the competing interests from each stakeholder as I was able to empathise with each of them on a much deeper level than before. I feel this contributed to the success of the project and gaining early buy in from all parties.
LEARNERS ENJOY COMMUNITY, NOT A FANCY LMS
Initially, I was disappointed with the software and technology available to create the end product; however, as I tested the course with the early users, it became evident that the content was much more critical. Building a community around the learning was much more important than prioritising the online development of the course.
Moving forward, I will now be looking for opportunities for participants to interact with other learners and create a sense of community despite it being a virtual learning experience.
